|
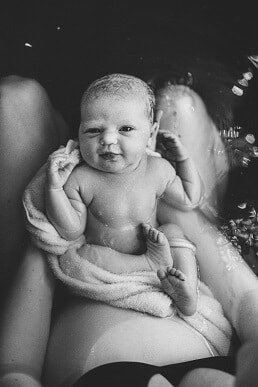
The story of Stella’s journey into the world really begins with her big sister’s. Florence was born via emergency caesarean following a cascade of interventions after an unnecessary and unwanted induction. I started researching VBAC before I’d even left the hospital. After the educational journey I went on, the idea of going to hospital as a healthy woman with a healthy baby to give birth seemed insane and I knew I wanted a HBAC. The evening of 41 weeks, after five weeks of relatively painless prodromal labour, I had my first painful contraction. Another followed within about five minutes, and it was on. Over the next few hours, I set up my birth space while bouncing on a ball, TENS machine on and vocalising strongly with the help of my doula. I laboured about six hours before hitting a wall. My contractions had been feeling good and productive, but a new pain had developed like a thin, tight band pulling from my pelvic bone. I knew instinctively it wasn’t an emergency - just a signal that labour wasn’t progressing as well as it could. I pushed through, moving from the pool, to the toilet, to the lounge room. I couldn’t get relief from the intensity of that band no matter what I tried. After a strong and productive start to labour, I’d felt sure I’d be having a baby before sunrise, so as I noticed the sky lightening through the curtains, my resolve was faltering. My midwife arrived around 7am (my doula and photographer had arrived earlier in the night) and the sound of her keys jangling in her hand as she walked up to the front door made my heart swell with relief. She sat quietly next to me, spoke gently and watched me for a while. I decided on a vaginal exam, hoping to discover why I was stagnating. I was dilated to 7cm, but baby was quite high. My midwife kept her hand still while I had a contraction and informed me that I had a huge bag of waters that was going rock solid when I contracted, which was possibly why baby wasn’t able to descend. She also noticed that bub was pushing against the top of my pelvic bone during a contraction, explaining the tight band of pain I’d been experiencing. I was exhausted, but had a renewed energy with my midwife there and an explanation for how my labour was feeling. We tried a forward leaning inversion, followed by Walcher’s position and something to eat and drink before resting a while. I slept as best I could for a couple of hours, and then treated my neighbours to a show as I trudged the hill down our street in a short house dress, TENS machine wires poking out from behind my bum, adult nappy on to catch the bloody show that was still seeping out of me, mooing with each contraction, and doing abdominal lift and tucks with a rebozo with each surge. Despite everything, my contractions spaced out further as the day went on. I had a hail mary visit to the chiro in the late afternoon before surrendering to a hospital transfer with contractions now fifteen minutes apart. We were fortunate to be allowed two support people, I’m not sure how I would have managed otherwise. Having my midwife felt like having a shield against the system, and we were lucky to be treated with respect and kindness. When we were taken into our birth suite, I appreciated the hospital midwife’s hands-off approach. We requested an artificial rupture of membranes, which hadn’t been safe to do at home but which we hoped would clear the path for my baby’s head to descend. The exam preceding the AROM was awful. The emotional exhaustion was catching me up and I was having to face the reality of the hospital transfer and all that comes with it. I sobbed my way through the VE, tears running down my face as my dear midwife gripped my hand and held her other hand to my cheek and my husband stroked my hair. The hospital midwife broke the waters and she felt the head descend slightly. I laboured for another couple of hours: sitting on the bed, standing and leaning on the bed, even in the shower. I was so exhausted that my legs were barely holding me up any more, but my contractions were so intense that I couldn’t sit through them. I was losing energy to vocalise, which was the only thing keeping me grounded. As strong as they were, they were still ten minutes apart. At twenty-six hours in, and the prospect of labouring for still many more hours, my desperation was mounting. I knew there was a real chance of a repeat caesarean now, and I asked for an epidural, hoping it would relax my body and allow me rest so that I could still give birth to my baby vaginally. I cried as I told my midwife and husband that I couldn’t keep going. I was sad, disappointed, scared and confused. I’d worked so hard for so long with all the confidence that my body and baby knew what they were doing and I just needed to work with them and power through it. Now, I was unravelling alongside my plan for a natural, peaceful water birth at home. Within the hour of getting an epidural, we were recommended a repeat caesarean. The doctor was lovely and respectful. After a frank conversation with my midwife discussing the risks, benefits, and the reality of our situation, I knew the right call was to go to surgery. I watched my delicious, gooey, chunky baby pulled out of my body and flopped straight onto my chest, and I moved her luscious, twisty cord to joyfully confirm my suspicions that she was a girl. We spent a few nights in hospital before returning home and reuniting with my eldest. I’m not alone in reconciling the complexity of a homebirth transfer and caesarean, and to all of us out there, know this: giving birth to a baby at home is not what makes you a homebirther. Our belief in the rite of passage of birth, and the respect for our right to bodily autonomy and informed decision making are what make us homebirthers. I believed so completely in my ability to have my baby at home, processing the fact that I didn’t has been a challenge. One of the hardest parts to accept is that I will never know why she didn’t descend. While I can speculate until the cows come home, I will never know. If I had another baby, I’d plan a HBA2C. I couldn’t walk into a hospital as a healthy woman with a healthy baby to have major abdominal surgery purely because of a couple of scars on my uterus. Plus, I reflect with such fondness on the relationships I developed with my birth team, and the care that they took with my family and me. My eldest still talks about “her friends” and plays midwife with her doctor’s kit. These women have left a lasting impression on us, and I will be forever grateful to them for empowering my journey to becoming a parent for the second time. About Katelyn I’m a married mum of two beautiful girls, Florence and Stella, living in Western Sydney. I used to be a person who said “I love the idea of a homebirth but it’s not for me” until after the birth of my first child when I experienced the maternal health care system and witnessed the way guidelines and policy fly in the face of evidence, and care providers are both inexperienced in assisting with and afraid of physiological birth. My subsequent educational journey has made me an aspiring birth worker and homebirth advocate. I am particularly passionate about supporting women in navigating their next birth after caesarean, and desire for every woman to be empowered with properly informed decision making in their pregnancy, birth, and postpartum. I have since trained as a doula and released a birth after caesarean mentoring program. You can find me at @thenbacguide on instagram or katelynthedoula.com.au
77 Comments
At 40+3, at 3am on the 3rd of July, the night/morning of the new moon, I woke to contractions 10 minutes apart. Speaking to my baby, I let her know that I was excited to meet her soon, asking that she go gently, that we work together to ensure she was born beautifully and gently, at home. Going to the bathroom, I took my last ever belly-selfie and listened to my hypnobirthing soundtrack. Back in bed I shifted through the discomfort and built a pillow fort to allow me to lean forward. Calm, but unable to rest, I got up to drink and wee several times. Every time I walked by the clock it showed repeated numbers – 3:33, 4:44, 5:55 – just as I’d seen throughout this pregnancy. I decided to get up and sat in my birth space, rocking back and forth with my forehead on the cold window. The space was beautifully prepared, both physically and spiritually – I could feel my tribe of women holding me in this space. Photo credit: Jerusha Sutton Photography "Call Jo!" (otherwise known as, 'call the midwife!') I messaged my midwife (Jo), photographer (Jerusha – Ru), and childhood friend/doula (Jacquie), to let them know I was in labour. By 8am I was moaning through 5 minutely contractions but easily able to chat between them. In order to ‘get on with the day’, like I so often suggest to the women I support, I went to the chiropractic appointment I had booked for 9:15am. The car trip was hellish – how women labour in cars beats me! After adjustment the contractions were suddenly closer together; two to three minutely, lasting 45 seconds. We went for a brief walk then travelled home with lots of stopping and me rocking and moaning on the side of the road. Juz was shaking his head asking, “Wasn’t the point of a home birth being at home? Why are we here!?!” Back at home, at last! By 10am I felt nauseous; I was working during contractions, but still fine in between! Juz was telling me to stop doula-ing myself! I asked him to set up the pool, maybe that would help me zone in? Jo rang and we chatted through a couple of contractions; we decided she should come and check on us, and we messaged Jacquie and Ru too. Jo and Tash (student midwife) arrived at 11:11am and Jo confirmed that bub was engaged and happy. Jacquie and Jacqui arrived soon after, both bailed up by our dog, Obi. Then Ru arrived. Everyone was here! But I was sure it was too early! I sat on the fit ball, Jo holding a heat pack on my back, Juz holding my hands/heat pack on the front. I felt so supported and loved! But I felt that this wasn’t doing anything! I sat and cried; big fat tears dripping onto my bare belly. “I just want to meet my baby!” Obi licked me, sitting by my side. I asked Jo why it wasn’t progressing; she suggested I get out of my head. I asked her with bitterness, “And how exactly do you propose I do that?” I don’t remember her response, the question was rhetorical. Photo credit: Jerusha Sutton Photography In the pool - ahhhhh I got in the pool and everything intensified further. I gripped Justin’s hands, Jo’s, Jerusha’s, whoever was there. Jacquie and my kids were so beautifully present, the kids wonderfully unphased – it was just another day. I could feel myself becoming transitional and decided I would doula myself through it. After what felt like an hour of this I started voicing my doubts. Frustratingly, my birth team had answers for everything, but they weren’t what I wanted! Photo credit: Jerusha Sutton Photography Transition... “How much longer?” “As long as it takes.” “I’m done!” “One at a time.” “I need an epidural.” “No, you don’t.” Each contraction felt worse than the one before! I needed a time limit, answers, SOMETHING! It was relentless. Willow (5.5yo), Hamish (2.5yo) and Juz were providing me water and massages. I was screaming, “Owwww, nooooo, noooo!” until Ru held my hand, massaged me and helped turn it into a “Yesssss-aaaa-owwwww!” I was getting grunty at the end of contractions – ‘Good, we’re getting somewhere!’, but the grunty urges never got longer or stronger. “Jo, can I just start pushing? I need this baby out!” Jo suggested I see if I could feel baby’s head. I reached into my vagina and couldn’t feel anything noteworthy; just a squishy mess. “Where is this bloody baby!?!” I cried. and some more transition... I was so tired. Jo and Ru guided me to totally relax between contractions and I started ‘falling asleep’ over the pool side. Ru fed me a bliss ball and some honey and lemon tea, but I still had no energy. Jo got some Clary Sage on a tissue which I asked her to take away. A few contractions later I smelt it again, “Get it out of here!” I yelled. ‘I know what you’re trying to do, Jo!!’ Willow showed me a card she’d made for baby – it was so sweet, but I couldn’t acknowledge her. Photo credit: Jerusha Sutton Photography and more, just for good measure! I was done; I asked Jo what we should do. I’d been in transition for what felt like days! Jo mentioned she could check where we were at. “Yes, let’s check!” As I stood, some bloody show came out – ‘Excellent! That happened when fully dilated with Hamish, this’ll be the same!’ I waddled into the bedroom believing I’d be 9‑10 cm. But I was 7 cm (Jo added I was stretching to 9 cm, apparently I blocked that out!). I despaired – this was too much! Jo reassured me it could go quickly from here, “Let’s just keep going.” I got back in the pool, hating the world, angry at my body, screaming I’d done this before and could do it again! “Come ON baby, go gently!!!” I kept glaring at everyone through weak, cruddy contractions. My mum rang but couldn’t get through, so dropped by. I’d debated whether to have her there, now I was being given the chance to decide. I knew this was too intense for her, it felt too intense for me! I let her be sent home. Photo credit: Jerusha Sutton Photography Come ON baby!!! I needed to wee but couldn’t. Jo suggested I try visualising my waters breaking on the toilet. I sat backwards on the toilet, bashing my head on the tiles, visualising an explosion of waters…nothing. A pop?…nothing. A trickle? Come on!! I did a tiny wee; STILL no waters. I sat in the shower on the fit ball until the water felt cold, still no waters. I got back into the pool, deflated. I’d told myself, “I’ll be holding my baby tonight,” but it suddenly got dark (the rain settled in) and I questioned this! Photo credit: Jerusha Sutton Photography I was convinced my full bladder was holding everything up and asked for a catheter; Jo agreed. I HATE catheters, but luckily my midwives are super-human and I couldn’t feel it once in! It did nothing. After a few contractions, feeling like I was dying without the pool, I asked Jo to break my waters; something needed to shift bloody soon! I screamed through brutal contractions on my back as Jo broke them; immediately everything shifted gear. I was FINALLY dropping into my body now, though I had an anterior cervical lip. I got on my knees with my bum in the air while Hamish sat next to me eating peanuts! “Geez mum!! You sore?” he asked. Willow announced, “There’s blood EVERYWHERE out there!!” Please come out now! I was asked to try 20-30 minutes of contractions without pushing; cue horse‑lips, screaming, tantruming and kicking and punching the lounge! I calculated (still in my head, then) that 20 minutes would around 5 contractions; I did 4. Constant words of encouragement were everywhere now! I asked for the catheter to be removed. “Jo, can you check again?” Surely this was almost over! The lip was still there. “I can’t DO this anymore!” I wanted the pool! More screaming, horse-lips, bum-in-the-air contractions and I started involuntarily grunting at the end. The next contraction, despite doing horse‑lips, my body pushed! “I NEED THE POOL!!” I hopped in, collapsing to my knees. Relief! Then the next contraction came and so did babe’s head – whoa!! I heard Jo ask, “Is that bub’s head?” “Yep.” “Ru, get in here!” The first hello I tore birthing Hamish, so had asked around about how I could avoid it. As a friend suggested, I felt bub’s head descend while rubbing my perineum – That squishy scalp felt incredible! In just one contraction I breathed my baby out. “Ha-ha-ha,” down, down, down…pop! Bub did some acrobatics and with a tiny tightening she wriggled and slid into my hands (a tiny tear!). I turned over and slowly brought our baby into the air – Just as I’d hoped. The kids were looking on excitedly. Suddenly, everyone that needed to be here was. Photo credit: Jerusha Sutton Photography Jo and I untangled bub from her cord, and then she did the ‘Sing‑baby‑thing’ and went floppy. It took some rubbing, suctioning and bagged air, but she let out a cry. I felt the cord pulse – our connection, it was amazing!! Willow asked Juz, “Is it a girl!?” “Yes!” She was SO excited! As soon as bub was breathing she pooped and latched on for a feed! Photo credit: Jerusha Sutton Photography Home birth! An extraordinarily ordinary day! I wanted to birth the placenta in the pool, but had to get out for the bleeding. I waddled to the lounge. Hamish watched closely (“Whoa, mum!”) as I birthed the placenta with some gentle help from Jo. I ate toast and honey tea as I soaked in the beautiful bub I’d just birthed, surrounded by the love and support of my incredible birth team. Jo measured Evalie and tied the cord, Willow cut the cord, Hamish cut our mother’s blessing bands and then we ate birth‑day cake that Jacquie made with the kids while I laboured. We dressed Evalie and I showered (no pain!) and got into bed. Everyone said their goodbyes while Jacquie brought dinner. The kids were so overtired and excited! We chatted through how I felt and I couldn’t stop beaming – I was so proud, happy, and in awe of our perfectly complete family! Photo credit: Jerusha Sutton Photography Thank you! I’m so grateful I had the opportunity to birth a little girl with such power into such love. I’ve never felt so held, loved and supported! I am so grateful to have been surrounded by such a delicious group of people; the J‑team (Jo, Jacqui, Jacquie, Jerusha and Juz), Tash and my kids. Thank you to all of you! Thanks especially to Jo and Jacquie, who have supported us through all of our family’s 6 pregnancies and 3 births, who introduced me to home birth, creating what I’m sure will remain a lifelong passion, and who have both sacrificed countless hours with their own families to support us. We are eternally grateful. Thanks for reading if you managed to get this far! If you’d like to hear me tell this story I speak about it and my previous two births on the VBAC Homebirth stories podcast and the VBAC birth stories podcast! I also speak about my first two births on the circle of birth podcast! You can also read about Willow’s birth story here and Hamish’s Homebirth After Caesarean here. About Aimee
Hello, I’m Aimee! I support women and their families through pregnancy, birth, postpartum and breastfeeding. I am a qualified and experienced Doula and lactation consultant, providing support in the Blue Mountains and surrounds. I am also a Calmbirth educator and President of Homebirth NSW. I’d love to meet you for an obligation free catch up! Contact me here. It’s hard to know where to start, but I suppose I’ll start with my pregnancy. My pregnancy with Logan was great! I felt fantastic until around the 36/37 week mark when my feet started swelling. It became quite uncomfortable but I was still as active as I could be, spending lots of one on one time with Maverick. Photo credit: Life and Lens Photography I was not expecting to go to 40 weeks as I had Mav at 38+4 spontaneously! But as the days and weeks went on, I had to find a way to let go of that expectation. I listened to the Hypnobirthing Australia tracks every night - Surge of the Sea, Rainbow Mist and Baby, Come Out. I would have quite intense, consistent surges between 3 and 6am for about 8 days before I actually went into labour. I spoke to baby a lot, especially in those early hours of the morning when it was quiet and we were alone. I told him that I was ready when he was! I had to practice so much surrender. Matt ran me lots of lavender and clary sage baths, I did meditations and chatted to bub in the bath as well. I had some amazing cuddles with Matt and with Mav. Mav talked to baby and baby would kick him in the back while we cuddled which Mav absolutely loved. On the 13th March in the late afternoon, I started to have consistent surges, between 5 and 10 minutes apart for a number of hours. I called my team. We all expected things to move quite quickly as my labour with Mav was only 5 hours. My midwife, Jacqui, doula, Aimee and photographer, Sarah arrived at around 8pm. I was going between bouncing on the ball and leaning over the lounge. When I stood up though, my surges spaced out. The birth pool was filled and I got in. The relief was instant. The water was amazing. I had my birth playlist playing, reading my affirmations on the wall and having my husband pour water over my back and my sweet Maverick rubbing my shoulder. Aimee was keeping me well hydrated. My pain was significantly less when I felt Matts hands on me, it made my skin tingle. When I got in the pool, my surges slowed to every 10-15 minutes. Maverick went to bed and I felt very emotional. I felt guilty that he would have to share me and that our relationship would change. I cried. Photo credit: Life and Lens Photography At about midnight, Jacqui told me she thought that babies position was causing my consistent contractions but I was still in early labour and that I should head to bed and try and get some rest and that she would drop by in the morning to check on me. I jumped into bed with Maverick and had lots of cuddles. My contractions eased and I had a great nights sleep. The next day I called my acupuncturist who generously said that she could make a home visit for me. Angie came and gave me a wonderful, INTENSE, treatment. I felt my baby kick like mad! It was very relaxing. On the 17th March surges started strong and consistently at about 7pm, just after dinner. These sensations were much stronger than before. I went to bed with Maverick, with the mindset that my baby was never going to come. I was 40+3 at this stage having had days of prodromal labour. I was already exhausted. I was awoken at 11pm with intense surges only a few minutes apart. I stayed in bed for a few hours, breathing and cuddling maverick. I got up at around 2am and woke Matt, telling him that it must be time, that it really hurts and I was going to get into the shower. When I stood in the shower, the contractions didn’t ease as they usually did. They were intense, toe curling, I moaned. I roared. Matt called my birth team again and they arrived at around 4am. They filled the birth pool again and I got in. Once again, the water provided such a huge relief. I swayed and moaned, vocalisation helping immensely. Maverick got in the pool with me and rubbed my belly. My surges slowed again, so I got out and leaned against a chair. I felt a trickle of water down my leg and said that I thought my waters may have broken, but wasn’t sure as it wasn’t a gush like it was with Maverick. Photo credit: Life and Lens Photography At around 8am, everything slowed again. I asked Jacqui for a vaginal examination because I was so defeated and needed to know what my cervix was doing. I was 2cm dilated. I wasn’t upset or disappointed with that as I dilated very quickly with Maverick. We decided to send Mav to preschool, Matt to work and I was going to go back to bed to try and get some rest. Aimee and Jacqui were going to get some breakfast to hang around close to home in case anything happened. I slept for about 2 hours and was awoken at 11am with intense surges 2-3 minutes apart. I tried to rest between surges and listened to my Hypnobirthing tracks, but I could not concentrate. My mother in law came around midday and brought lunch. I couldn’t eat, but had some coke for some caffeine and energy. My surges consistently stayed at 2-3 minutes apart if I was standing or upright, or 10 minutes apart if I was lying down. I stayed lying down in bed to get a break and attempted to get rest, but it wasn’t happening. At around 1:30pm the sensations changed. I knew immediately that baby had moved into a full posterior position. I called my chiropractor. She described a number of manoeuvres to try and ease the sensations and texted me some photos. My mother in law did these manoeuvres and they worked fairly well for a while. At around 2:30 I messaged Jacqui and told her, “I don’t know how much longer I can do this”. She called soon after and helped me to relax, telling me that my body was doing exactly what I had to do to bring my baby down. She said I should call Aimee but I was still in denial that baby was coming and I didn’t want her to travel all the way down the mountain to have to go all the way back for the third time. In retrospect I definitely should’ve called! Matt got home around 5pm with Maverick. At this point I was feeling very sorry for myself. I was crying, I felt defeated. I was staying on the bed because I was getting a slightly bigger break between surges. At this point they were painful, and I feel that they were more painful due to my extreme exhaustion. Matt was doing hip squeezes during surges and putting counter pressure on my back. It must have been frustrating for him because it was never the same spot that provided relief! Maverick was happily playing in his toy room, coming in every so often to tell me I was being too loud! From this point, things got quite blurry. I lost control a bit… no. Actually, I lost control a lot! I had a bloody show at around 6pm. This was SO exciting. It was something different, progression! Matt messaged Jac and she called and was also very excited. She heard that I was distressed and said she would make her way over. I think she got to our house around 7pm. When she walked in, I told her I wanted to die. I told her I was in fact dying. “No sis, you’re not dying. Let’s hop up and get into the shower”. So I got in the shower around 7:30ish. I tried to stand, but couldn’t at this point. I was then on all fours and I threw up. Jacqui was sitting on the floor in the doorway telling me that I was doing great. She said that she was going to unpack her things and call Aimee. I cried and told her not to unpack her car because the baby was “never going to come”. She said, “Jaime, we’re not leaving without a baby tonight!” I repeated this in my head multiple times and it helped immensely. Aimee arrived at about 9pm and I believe this is when Sarah was called. I was back on my bed, really out of control. I was saying that I felt like I was dying. I told Matt I couldn’t do it anymore and true to his tough love style, he said “well we can go to the hospital and they can cut him out?” I needed that reality check! He never faulted. He was exactly where I needed to be at every turn. He never freaked out, not once did he ever question me or my ability. I felt such a huge relief when Aimee arrived. Logic and calm. Matt continued to do counter pressure and hip squeezes while Aimee offered me water and kind words of encouragement. I was using acupressure points on my hands when I remembered to as well which actually worked quite well. Aimee asked if I wanted her to call Sarah, our photographer. I said no because it was probably still too early. *it wasn’t. At some point Mel, my second midwife, arrived! I asked for another VE and I was 5cm dilated. I asked Jac to break my waters. I really felt that this was the barrier to me progressing even though logically I know that’s not the case. Jac asked if I was sure and asked if I wanted to wait a bit longer. I said no, that I wanted her to break them now, that I couldn’t go on like this any longer. I went to the bathroom, came back and lay down to have my waters broken. I was 7cm and my waters had already released, so they had broken that morning. I truely believe that I had a mental block, thinking that my waters were still in tact. Once I knew that they weren’t, everything changed. I wanted a completely undisturbed birth, but having a team that I completely trusted and knew, made me comfortable asking for these interventions. At this point I walked out to the dining room, my contractions taking my breath away. Matt held me and Jac told me to breathe. I couldn’t, it felt like I couldn’t take a breath in. I was on my toes, the pain in my back was intense. I was trying so hard to breathe but at this point I just felt high. I felt out of control and like the room was spinning. Everyone’s voices were distant and echo-y. Jac suggested going to sit on the toilet. I went and sat on the toilet with Aimee, while Matt tried to get Mav to sleep. We definitely didn’t expect things to move this quickly. I had actually accepted that my baby was NEVER going to come. It sounds crazy, but I literally accepted that I was no longer going to be alive. I felt really calm at this point internally, no too sure about externally. I surrendered. Photo credit: Life and Lens Photography I had one contraction on the toilet which was very strong. Then another and I felt my babies head drop. I started to get the urge to push. I couldn’t speak or think. It felt like the world was spinning and everything was in slow motion. I was aware that Sarah hadn't arrived yet, but at that point I didn't have the energy or the focus to care. I'm very thankful though that Aimee took lots of video and photos! Aimee called Jac over and they helped me into the pool that someone had filled. I called out for Matt who was still trying to get Mav to sleep. Matt grabbed Abby and Mav and brought them to the pool. The pain eased immediately as I got in the pool and knowing that my family was around me made me feel safe and excited. The next contraction, I felt like I was doing the biggest poo of my life. It had to be poo because as I said, I had accepted that my baby was never coming. I felt the familiar stretching of my perineum, it’s not something you forget. My babies head was born at 10:08pm. I reached down and felt my babies head, with lots of hair! I felt so much relief. I knew that I would meet my baby in the next few minutes and I was so excited and ready for my back pain to stop. Feeling his head was surreal. I longed for that in Mavs birth but it was railroaded. Even now when I touch Logan’s head, I’m taken back to that moment. It makes me so emotional! The next contraction, I pushed the rest of my baby out, receiving him into my own arms. It was the most surreal, amazing moment. Overwhelming relief was what I felt. The pain was gone. I finally had my baby even though I was convinced he would never ever come. And I was alive. I cried. And cried. And cried. Photo credit: Life and Lens Photography Maverick got in the pool with me, Matt stroked my shoulder and Abby watched on. It was absolutely amazing. Looking at my beautiful baby, he was not what I expected. I suppose I expected to see a little Maverick, but he was a completely different little person. I looked for Maverick immediately and he was already bigger than he had been hours earlier. The look of adoration and love on his face still brings tears to my eyes. I will never forget the look on his face as he met his baby brother. Maverick said, "you are beautiful mum" which just melted my heart! For weeks afterwards he would randomly say "mum is so strong and beautiful". It was at this point I felt myself coming back into my body. I realised that I was in the spot that I had sat in my mother blessing a few weeks prior. How powerful to have all the candles from my tribe in eyesight, all my affirmations. Just the feeling of being held, even from afar. I still have my birth alter set up today and don’t see me taking things down anytime soon. Matt FaceTimed my mum and I spoke to her for a couple of minutes and showed her our new baby. About 20 minutes after Logan’s birth Jac asked if we minded cutting the cord, getting bub skin to skin with dad, birthing the placenta and getting baby fed. He was very, very small and a bit congested so we just wanted to make sure that everything was ok. About 5 minutes after that, the placenta was birthed, completely naturally. I felt some stinging and assumed that I may have some tearing. Photo credit: Life and Lens Photography I got up and felt empty. It was a sensation that I don’t remember feeling with Maverick. I felt completely hollow and it made me feel sick. I made my way to the couch and held my baby to my chest and he began to feed. Once again there was so much relief that I wasn’t having any pain. Sarah arrived around this time. She saw me on the lounge but continued through to the birth area and saw the others emptying the pool. She said that she thought it was another false alarm until they told her I was on the couch with the baby! I was so ravenous all of a sudden. Someone made me vegemite toast and it was the most amazing meal I’ve ever had! Photo credit: Life and Lens Photography Baby was fine, just very small. Jac gave us a tour of the very cute, small placenta while I ate all the food. I think I had the toast, 2 muesli bars and an apple in about a 5 minute period. Jac checked to see if I had torn.. not even a graze! Baby was 2.5kg and was 48cm long! It was so amazing to be surrounded by the people I love and to be in the comfort of my own home. The next few hours were simply bliss. Matt took Mav to bed, Abby went to bed. My mother in law went home. Jacqui and Mel put down the pool and packed away their stuff. I sat with Aimee and Sarah for another hour or so and talked about everything that had just happened. It was so beautiful, just being with women in that space. My birth was not what I had planned for or what I had expected. I feel that I was in my own head quite a bit, overanalysing. The support of the people around me though, grounded me, even momentarily. I do not have any regrets about the choices I made because I know that they were the best choices for me in that moment. I never felt pressured into anything! Our little Logan showed me that I have strength and courage that I never thought I had. He showed me patience and love that knows no limits. It was empowering and painful and transcending and staggering. It obliterated every part of me and then just as quickly made me whole again, expanding my heart in the process. It was birth. My name is Jaime Leigh Hawkins, I’ve just turned 30 and I am a wife, mama and step mama. I am a doula (This Is What I Doula) and I also teach the Hypnobirthing Australia program. I had my first son, Maverick, in hospital 4 years ago and had a less than fabulous experience. I decided at the last minute to have my placenta encapsulated and I connected with a local doula. After birth, I researched more about this term, “doula”, and it was like a lightbulb went on. When joining the doula world, I learnt so much about homebirth and knew that for my next baby, I would birth at home. Are you a member of Homebirth NSW but unsure how to access our members-only content?
Here's what to do (click here to watch a fly-through of this process):
It is with great sadness that we advise our members of the passing of Akal Khalsa, a dear and treasured midwife, long time support and one of the founding members of our organisation. Akal was an incredible asset to the homebirth community and she will be dearly missed by our community, her friends and by her daughter, Pritham Khalsa, and grandchildren, Jasmine Sherlock, Kaha and Mārū Packman and Forest Khalsa. Below are some words from those who knew her personally. Jacqui Wood I met Akal when I first arrived in Sydney in 2006. She was a long standing private midwife and word about town was she could ruffle feathers. With this information, I knew we would be friends and we were the best of friends up to the day of her passing. As an elder woman and midwife, she was my friend and mentor and was always there with down to earth advice. We came from very different generations of Midwifery practice and not all of her advice I would take on. She once looked at me very seriously and said, “Now Jacqui, do you get your ladies to prepare their nipples for breastfeeding?” I told her, I did not; she looked at me sternly and informed me this was something she always did and advised me to consider this in my practice. Suffice to say, this is not something I have taken on. In her retirement, she moved to New Zealand to be with her Daughter Pritham and 3 grandchildren; Kaha, Mārū and Forest. She had just completed the ski season for 2021, attended pilates regularly and had taken up bee keeping and was an active member of the bee-keeping group. She was very happy and thoroughly doted on her family. I think of her now reunited with her son, Raj who passed away in 2010. She will be looking down at me telling me to dry my eyes and stop being silly. I loved her dearly and will miss her terribly. Goodbye my love. Maggie Lecky-Thompson I am sad to hear the news of Akal’s passing. My only real peer in Australia. Starting our practices in 1978 as homebirth midwives in Sydney, from very different backgrounds and varying in our approaches. Akal was such a fierce mother for the women who were her clients. In the tiredest of times when I needed another brain to work through a situation at a birth I would call her and we would talk it through. She did the same with me. Akal did me the honour of asking me to be her midwife when she became pregnant with Raj Gopal Singh. It was a lovely birth. Tragically, 11 years ago Raj was killed in a catastrophic road accident. Akal called to tell me the news. I’m glad that we were able to connect and see each other and talked about Raj and the next steps in our lives. Akal believed she would be with her son after her death and this is where I see her now. Robyn Dempsey Akal was one of the most fierce and forthright midwives I’ve ever met. To be honest, I was a little afraid of her! It wasn’t until I had birthed my third baby that I actually saw her the way her clients saw her. I was not one of her clients, however, at our midwife meetings, Akal showed me such tenderness, and concern, I was blown away. The way she made me feel will always be in my memory. I don’t believe Akal had an easy journey in this life, but she was an asset to women birthing at home for over 40 years. Akal, you will be missed, and forever in the thoughts of women, whose lives you touched during their birthing journeys. Cecily Greval Akal was one of the few home birth midwives in Sydney in 1994 when I approached her when I was pregnant for the first time. I immediately liked Akal as she was direct and straightforward informing me that if I didn’t plan to breastfeed, she wouldn’t assist me. I valued her honesty and truthfulness. I will always be grateful for the care Akal gave me. My waters broke many hours before labour. Akal arrived immaculate in her white dress and matching white turban as usual for her at that time. We decided to transfer to the hospital due to the colour of the waters. Akal stayed by my side and was my constant advocate during my labour. I can still clearly remember her stroking my shoulder and sweetly advising me during this process. She remained with me for some time after the birth and in the days that followed helped me with breastfeeding. With her finger she invisibly wrote “SHOULDERS” on the wall to remind me to relax when feeding my precious newborn – this memory still comes to mind when I am tense. I have nothing but gratefulness to Akal for her midwifery skills and her care of me and my tiny newborn. She was forthright, strong and defended mothers like a lion. I felt a great loss when I heard of her passing which was all too soon. She paved the way for other midwives and women who wanted home births. Vale Akal.  Homebirthing during COVID, reasons for transfer and the benefits of the unparalleled standard of continuity of midwifery care. Welcome to our Homebirth NSW blog! This edition is all about some of the fantastic questions asked during our Midwife Q&A live event. Our aim is to create blogs covering many of the questions so that answers are not only easy to find online, but quick and simple to share with anyone such as birth partners, family members and friends. This way, if you are planning a homebirth or hoping to educate a birth partner or family member, you can simply read and share answers straight from the incredibly experienced and knowledgeable private midwives themselves! It’s important to note that although many privately practising midwives work within similar parameters, they are autonomous and can only speak for their own individual practise so some answers may vary between midwives. A HUGE thank you to Jo Hunter and Janine O’Brien for taking the time to be a part of this event and answer so many questions about homebirth! As the author of this blog, I’d like to acknowledge that I am using information shared from Jo and Janine in the live Q&A which can be found by clicking this link. Let’s dive in! Question: Has COVID changed anything you need to do re homebirthing? The short answer? Nope! The only changes are those that have been highlighted for the general community such as being more vigilant with hand washing and mindful of possible symptoms. The amount of support people is the woman’s choice and at her discretion. As Janine states, “often what makes homebirth special is not having people coming at you wearing masks and plastic”. Having a homebirth in a pandemic has the added benefit of being free of hospital policy in regards to masks, support people and of course avoiding the many infections and bugs that reside in hospitals even when a pandemic is not upon us. Question: What would be the reasons for transfer to a hospital birth during pregnancy or during labour? This is such a good question! Most families planning a homebirth will want to be aware of anything that might mean a change of plans in regards to birth place. During pregnancy, circumstances arising such as preeclampsia, placenta previa (the placenta covering the cervix), known breech position or twins might be some reasons for transferring to a planned hospital birth. Private midwives are experts of physiological birth, and as such they are highly skilled at recognising when labour is deviating from normal, even more so because they know the women they support on a deep relationship-based level and will very likely notice anything that’s moving away from what might be normal for that individual woman. Reasons for transfer might be fetal distress, prolonged rupture of membranes, choice for pain relief, or thick stained meconium. Transferring for immediate medical assistance is incredibly rare. Jo Hunter states in the Q&A that she has a 7% transfer rate, which gives a pretty clear picture on how often it’s necessary given the majority of this percentage is not for urgent reasons! Of course, women are not choosing to have a homebirth at all costs, and in fact having continuity of care with a known midwife creates a relationship whereby women are safer as their care provider knows them individually and will only suggest interfering with normal birth when truly necessary. Which leads us to the next question! Question: What is the biggest difference between hospital and homebirth? Aside from being in your own home with your pets, your own bed, no bright lights or noisy chatter in your birth space that is? Easy, continuity of midwifery care. Accessing this type of care in a hospital is possible, yet it’s attached to many, many policy puppeteered strings. Having a privately practising midwife means your midwife has the autonomy to support women who would otherwise be ‘risked out’ of midwifery care or choosing a homebirth through a hospital program. When a midwife knows the woman, and the woman knows her in a genuinely caring and supportive relationship, that woman is going to feel able to let go and trust her birth team during labour. Having a hospital birth usually means that your midwife is whoever happens to be on shift that day, so it really is luck of the draw. And even then, shifts end and change over happens, bringing yet more new faces into your special birth space. Planning a homebirth with a known privately practising midwife means you really are choosing who you want to be there based on who you connect with, feel safe with and feel at ease with. As Jo refers to in the Q&A, all great hospital initiatives have been derived from the homebirth model. Men at birth, siblings at birth, water birth, the environmental factors; all happening at homebirth long before hospitals caught up. Of course, homebirth with a private midwife isn’t always feasible for women, that’s why here at Homebirth NSW we do what we do, advocating and spreading awareness so that one day all women can have all choices at their finger tips! Author of this blog: Claire Heenan Photo credit to Rebecca Lawrence  What made a midwife, an actress, and a doula/birth photographer decide to come together and make a documentary about Australia’s maternity system Good question. If we skipped to the end of the article the answer would be… care. Three women who knew what the gold standard of care is for pregnant and birthing women… and between them having delivered it (the care, of course, not the babies- they were birthed), having been on the receiving end of it, and in my case, as a doula, having witnessed all of the alternatives. Rewind to 2008 when Jo Hunter co-organised the Sydney Homebirth Conference and the Australian premiere of the documentary, the Business of Being Born (BoBB). Whilst the BoBB was a game-changer of a film, it was American and therefore a lot of people dismissed it as being irrelevant to us. Creating an Australian birth documentary was an idea and a pipe dream in her head. Fast forward to about 2015 when Jo and I met and became friends, she told me of her idea and showed me a homebirth film from the 1980’s called Labour of Love. The film was funded by the ABC and was a quaint, simple and quite delightful film which followed three homebirth midwives in Sydney and the Blue Mountains. It seemed like such a good resource to share in regards to birth, and particularly homebirth, but as lovely as it was, it was very dated (including lots of lovely pubic hair!). So we started dreaming of the possibility of making Labour of Love II. A current, Australian birth film. We went so far as to get permission from the filmmaker to do this (although she was slightly bemused that we wanted to go to the effort of making a homebirth film - having been there herself and knowing the time, money and effort that goes into such a thing). We became a little perplexed by how on earth we would go about making a film between the two of us, so the idea remained a dream. Later that year Zoe Naylor booked Jo to be her midwife for the birth of her second baby in 2016. Zoe had birthed her first baby in hospital and this time was looking for care with more depth. A little closer to the birth Zoe also called me - as she had decided she wanted to have her birth filmed. She was germinating an idea about a TV series and wanted to have the footage available to use for that. The birth team was set. Zoe’s birth of Beau was a magical evening and she was astounded by how different she felt having received true, one to one continuity of midwifery care. In the conversations that followed, Jo showed Zoe The Business of Being Born, and told her of our dream to make an Australian birth documentary. Zoe was in. Together we decided it was time to find out why so many women were coming out of their births traumatised, why birth related PTSD is on the rise, and why we have a postnatal depression epidemic. At this stage I was in the second trimester of my first pregnancy, so what better trio to start making a documentary - a newborn mother of two, a pregnant woman and one of Australia’s busiest homebirth midwives. The urgency was real. The mission became clear...to ask the question- what would it take for women to emerge from their births physically well and emotionally safe? I had cameras which were enough to start filming, so we bought sound and lighting equipment, learnt where the ON buttons were and hit up Hannah Dahlen to be our first interviewee. By this stage I was 35 weeks pregnant and Beau was 4 months old. Our timing could not have been better… in two weeks time the Normal Labour and Birth Conference was coming to Australia, and Hannah was organising it. Jo and I were to be attending the conference and after her interview Hannah said, “If you’re really making this documentary you need to make the most of these people being in the country. I will connect you with anyone you want.” We flew into action, Hannah played cupid and we found ourselves for the entirety of the conference in a private room, with the likes of Lesley Page, Sheena Byrom, Soo Downe and Melissa Cheney rotating through to share their expertise. This was October 2016. One week later I gave birth to my first baby, at home, with Jo as my midwife. Hands down best day of my life. We had about a 6 week hiatus and from there things snowballed. We were back at it-interviewing whoever we thought could lend their opinion to answer our burning question. We fitted these filming sessions in between birthing women, young families, running businesses, writing a thesis, speaking at conferences and many, many other things. We spoke to the likes of Sarah Buckley, Rachel Reed, Rhea Dempsey, Nicky Leap, Pat Brodie, Andrew Bisits, Andrew Pesce, Kirsten Small, Jane Hardwicke Collings, Sheryl Sidery, Bashi Hazard as well as following several women in their pregnancies and births both at home and in hospital, and interviewing many other women and partners. We travelled with our babies in tow, often with one of Jo’s teenage daughters with us to look after the little ones whilst we filmed. We breastfed through interviews, filmed women sitting on their beds with our babies lying asleep next to them, just out of frame, and conducted interviews in Air BNB’s after bedtime with the kids asleep in the next room. Again, the urgency was real. During this whirlwind of interviews, we met Olympian Selina Scoble while in Brisbane. Initially we interviewed her for her story as a 40 year old first time mother with various risk factors, and how she was being treated in the system. But our relationship with Selina quickly escalated and she became a key member of the Birth Time team. She is our behind the scenes goddess who is constantly tinkering away at all the little unseen things- our emails and website, accounts and merchandise as well as helping to plan and execute our next big moves. Our filming took us to some incredible places, none more incredible than to Alice Springs in July 2018. By this stage our babies were old enough to be left with their fathers for a few days so we jetted off to Alice with the two co-chairs of the Birthing on Country Project- Mel Briggs and Cherisse Buzzacott, to film the story of these two women working together, and to visit Cherisse’s home country. We also started hosting live events, as a way of bringing the birthing community together to boost education, moral, and a sense of togetherness. We have hosted three events to date - Feminism and Human Rights in Childbirth with Hannah Dahlen and Bashi Hazard, An Evening with Rhea Dempsey, and Birthing on Country with a panel of the key players from the project. All of these events are available to watch online through our website. Early 2019 after over 60 interviews, we decided it was finally time to draw a line under the filming side of our project and start to carve this body of work into something digestible. It was decided that our beautiful friend and honorary sister Ryan Harrison and i would take on the first pass of this mammoth task. Ryan and I spent the next 5 months locked in his studio bachelor pad with his dog, Biscuit and lots of dark chocolate, watching and scribing every single interview, and pulling together themes and threads which ran through 2.5 years of interviews. At times it felt like an insurmountable project, but by the end of the 5 months we had a 1 hour 45 minute film which was so dense with information, it felt like being hit over the head with a baseball bat. Simultaneously while this was going on, Zoe was on a fast learning track of the executive producers role. She threw herself into learning the ins and outs of the film industry from the angle of funding and government tax offsets- otherwise known as “how the hell you find enough money to finish a film”, because post production in films is the money equivalent of a postpartum hemorrhage. Since then we have agreed on, and then pulled out of a deal with a post production house, and as well as never quite agreed on and consequently pulled out of a distribution deal, all because we weren’t feeling respected and listened to, and they wanted more than we were willing to give. We have likened our experience to a birthing woman in the system more than once in this process. In October last year we revisited the hour forty five baseball bat of a film- Zoe, Jo and I locked ourselves away together for 36 hours and re-edited it to a much more palatable 1 hour 20 feature length documentary. We call Jo our Captain. Our chief breath taker. Whenever we need direction on something, whenever we need a decision finalised, we turn to her. Her wealth of knowledge having worked as a birth worker, activist and private midwife for over 20 years has been the bedrock of this project. Being held in such high regard in the birth world is what has given us access to the incredible array of people that have come on board our project. Through Zoe’s wizardry on the finance and relationships front we have landed ourselves in the incredible hands of Spectrum Films at Fox Studios for all of our post production, we have original animation and composition created by amazing artists, we have a new distribution deal and our film will be finished next month. And then comes the slightly heartbreaking part of the story- which someday we are sure will be viewed as simply a bump in the road… we were set to release our film at the end of April, tour the country with screenings and Q&A’s in 13 locations, and start the next chapter for what we have planned to change the landscape for birthing women. But alas, the world has ground to a halt. So, like any good midwife would, we sit with what is, not with what we want to be (thank you Jane Hardwicke Collings) and we wait for when this baby of ours is good and ready to be born. To stay up to date on all things “Birth Time” make sure you head to https://www.birthtime.world and sign up to their newsletter, get shopping or make a doantion.  Homebirth NSW How are you going? We truly hope you are well, safe and breathing a sigh of relief as restrictions ease a little. Been missing those cafe babyccinos? Maybe your kids have created SO MUCH ART and there's no more fridge door room for their creative genius. Well, good news, we want your kids' art! KIDS ART COMPETITION Is your child the next Picasso? Fancy their artwork being the cover of our next Birthings Magazine? Of course you do! What an incredibly beautiful keepsake it would be to have your own child's drawing, collage or painting of your family's homebirth as the cover of our timeless Birthings Magazine. Surely that's a future family heirloom, am I right?! Not to mention, the money we raise will go towards our efforts in advocating for ease of access to homebirth. It's all about intrinsic motivation these days, and what more reward would a kid love than having their artwork gain them fame by it appearing on an awesome magazine? Wait, maybe that's extrinsic motivation, oh well! Better than ANOTHER Bluey sticker book. All entries by gold coin donation via Paypal to [email protected] SUBMISSIONS BY 01 SEPTEMBER 2020 Send artwork to [email protected] Did you know that last week was National Volunteer Week? Here at Homebirth NSW, we are all volunteers who work hard and devote our time to changing the limitations and restrictions women face when it comes to choosing a homebirth. The theme of Volunteer Week was 'changing communities, changing lives'. The options available to families and the way women feel about their birth experience is foundational to building communities and changing lives! Homebirth NSW wanted to offer a huge thank you in particular to the incredible Virginia Maddock for her 11 (and a quarter!) years of dedication to our committee. As Virginia leaves our management committee, she has been presented with a lifetime membership with Homebirth NSW! Thank you so very much, Virginia, for: • taking on almost every different committee position at different times • attending and organising numerous rallies • being involved with sooo many Birthings magazines • running stalls at various conferences and events ...and much much more! Virginia runs her own amazing business too and you can check out all she offers here: Natural Beginnings - Holistic Health, Doula and Placenta Services. Our advertisers and partners - Your logo could be here! Advertising with us is a great way to support homebirth advocacy whilst reaching a wider audience for your business! To find out more about how you can become an advertiser, friend and/or sponsor, simply reply to this email and we will send you everything you need to know! Homebirth Q & A - We recorded it! Did you miss out on the amazing opportunity to listen in or ask your questions at our Homebirth Q&A session? Now you can check it out at whatever time works for you! We have it recorded and ready for you, just click here. Two highly experienced, wonderful privately practising midwives speaking all things birth in the comfort of your own home? Did your Sunday just get a million times better or what?! Join Janine O'Brien and Jo Hunter as they share some invaluable insights! Janine and Jo answer all the homebirth questions you could think of! I learned so much from listening to this! Thank you so much to our members for being a part of our community and supporting our advocacy work! We can't wait to see the beautiful homebirth artworks your kids create. Stay safe and reach out to us if you have any questions at all about homebirth and Homebirth NSW. Claire Heenan (Communications) Homebirth NSW
Your voice matters. Your experience in choosing where to birth matters. Your responses to our survey are a step towards advocating for what birthing families want. Have your say & help expand homebirth services nationally We have a game-changing, short survey live now, and would love it if you could add your voice. Please click here to tell us about your experience accessing and planning a homebirth in your area, wherever you are in Australia. Whether you ended up choosing a planned homebirth or not, your response matters! We want to hear from anyone who has actively considered a homebirth in the past, even if you didn't ultimately choose homebirth. We're interested in exposing the limitations and barriers to homebirth, as well as any perceived shortfalls of the hospital maternity system versus homebirth. We'll use the results to highlight the issues in our advocacy efforts, working towards more choice and more availability of homebirth for women and families in all parts of Australia. That's gotta be worth 10 minutes of your time, right?! By telling your story through surveys like this we hope to see:
Thanks for participating, your responses are deeply valued: click here! Claire Heenan (Media & Communications) and Kathryn Bell (Secretary & Intern supervisor) Birth is the labour of unconditional love. It is a transformative experience for both mother and baby. It is a time when mum has to go deep into her instincts and bring her baby into the world. It is the experience of a Goddess warrior.  Photo courtesy of Lora @rnr Creative Photo courtesy of Lora @rnr Creative After birth, the mother is in a very vulnerable state. Mum’s psycho-physiological state is as delicate as her newborn’s. In Ayurvedic medicine, it is explained that after childbirth the mother's physiology is going through a natural reset process to embody her ideal health for the years to come. It is a time when she needs proper support for her healing and rejuvenation to take place. Ayurveda is an ancient, holistic practise that has existed for more than 5,000 years. It is known as the sister practise to yoga. Yoga is the path towards self-realisation and ayurveda is the path of health and well-being. Together, these practises can bring so much love and harmony into one's life. According to the ayurvedic medical texts by the sage Shushrut, women are in an exceptional window for the first 42 days after childbirth (extended by ten days to 14 days if there was surgery). This window, also called the ‘Sacred Window,’ is a time where the mother's nervous system is like a flower; very delicate and sensitive to the environment. The sacred window is the time for the newborn mother to be nourished and nurtured so she can offer the most exceptional ability to love and serve her baby. It is a time for extended bonding with the baby and deep rest and rejuvenation. Why 40 days? "The first 40 days will impact the next 40 years to come" Ayurveda explains that it takes around 40 days for the essence of food to become Ojas (the juncture between consciousness and matter which is enlivening and regenerative), and for all of the seven tissues to be rebuilt properly (plasma, blood, muscle, fat, bone, marrow, and reproductive). After childbirth, this is the time for the mother to rebuild her tissues and establish health and well-being for the 40 years to come. What is mum’s Dharma? Dharma is one’s purpose in this life; one’s mission. The dharma of the mother is to go through labour to bring her baby into this world. After labour, it is mum’s dharma to nourish, protect, and love her baby. So in ayurveda, there is this special window to nurture mum so she can be there for her baby and serve them in abundance of love. What is happening during the ‘Sacred Window?’ During this time, mum's digestive fire is very depleted, creating difficulty in digesting food, life, and emotions. During and after childbirth, mum's body is experiencing different sensations such as pain, inflammation, and abdominal space. From the ayurvedic perspective, these all increase the ether and air elements within the body and mind, which can lead to mum feeling unsupported, bloated, empty, anxious, and with loss of appetite. What is happening with the hormones during this time? Right after birth, mum is filled with oxytocin and her heart with love. She is naturally radiating a divine glow. But around the third day postpartum, when the hormones drop and the milk comes, mum can start to feel overwhelmed, tired, and anxious. During this time, proper postpartum care is essential for the mother to have appropriate support and loving care. What are some of the practices to nourish mum? - Abhyanga: warm oil massage over the body - Belly binding - Ayurvedic herbs to enhance the healing process - Warm and nourishing foods - Rest - Warm showers - Sitz bath - And much love and care What is the benefit of Abhyanga and belly binding? Oiling the body in Ayurveda is called snehan. In Sanskrit, the word snehan means oil as well as love. It is the practice of loving our bodies and falling back in love with the God of our hearts. "This is a clear message of love, honor, and appreciation for your body" - Myrica Morningstar After childbirth, vata dosha (ether and air elements) is aggravated, and it needs genuine care and attention for the mama to have balanced health and to be able to recover and cultivate her strength. The oil recommended for the mother is black sesame or bala thailam (medicated oil) to help the nourishing, cleansing, and healing process. Belly binding is an ancient practice for postpartum mothers. It gives the newborn mother a feeling of groundedness and helps the organs come back into their proper place. Ideally, belly binding is practiced from the first day of delivery. For caesarean birth it is essential to wait so that the scar heals appropriately (4 to 5 weeks). What is the postpartum diet? Ayurveda has specific guidelines on mothers' postnatal diets. The food for the first three days should be peya (soupy rice) with panchakola (medicated) ghee and plenty of iron-rich sugar, low salt, and digestive spices. This food will allow mum's digestive fire to rest and reset. It will also give mum time to digest everything that happened and for her heart to fully connect with her baby. Ayurveda recommends slowly increasing the thickness of the food and gradually adding some cooked veggies, as well as some legumes like mung beans or red lentils. Ayurveda also recommends that the newborn mother must have warm spiced milk at night, which will help with the quality and quantity of breastmilk. For more information on Ayurvedic postpartum recipes check out “Healing recipes to Nourish the Newborn Mother” at www.soma-shakti.com.au. Mama’s spice milk recipe: Bring milk to a boil three times if you have the time with spices (cardamom, clove, black pepper, saffron, black cardamom and fennel; limit cinnamon until mother’s bleeding is under control), iron-rich sugar and a teaspoon of ghee (you can use oat milk instead of cow's milk). Final Word Food is one of the essential factors for mum to heal appropriately and for her milk supply to be consistent. A proper diet will also protect mothers from anxiety or postnatal depression. Currently, one in every seven women who give birth in Australia experiences postnatal depression. This a significant number of newborn mothers having difficulty in connecting with their babies and with themselves. A newborn mother needs to have proper support around her. I truly believe that planning a postpartum program is as important as a birth plan. If you are a pregnant mama, take your time to connect with different doulas and find the right postnatal care for you. Daniela Escobar is a dedicated and devoted practitioner of ayurvedic medicine and a yoga educator. She specialises in women's Health and postpartum care. She offers her services in Bondi - Sydney, and online. For more information visit her website. www.soma-shakti.com.au www.autismnaturally.com.au |
Details
Welcome to the Homebirth NSW Blog!
AuthorThere are various authors to our awesome Homebirth NSW blog, each article will specify the author. Archives
September 2022
Categories
All
|






































































 RSS Feed
RSS Feed